What You Need to Know About Angioplasty With Stenting

When the arteries that supply blood to the heart become narrowed or blocked, blood flow can be reduced, leading to symptoms such as chest pain or breathlessness and increasing the risk of a heart attack. In such situations, doctors may recommend a procedure called coronary angioplasty to restore circulation. Heart stenting is often performed as part of this procedure to help keep the artery open and support long-term blood flow.
If your cardiologist has discussed stenting with you, understanding how it works and when it is used can help you feel more confident and prepared. In the sections ahead, we explain how heart stenting fits into angioplasty, the different types of stents available, and the steps involved in getting ready for the procedure.
What Is Angioplasty and Heart Stenting?
Coronary angioplasty with stenting is a minimally invasive treatment used to open narrowed or blocked coronary arteries and restore blood flow to the heart muscle. It is commonly recommended for people with coronary artery disease (CAD), a condition in which fatty deposits, or plaques, build up along the artery walls and restrict circulation.
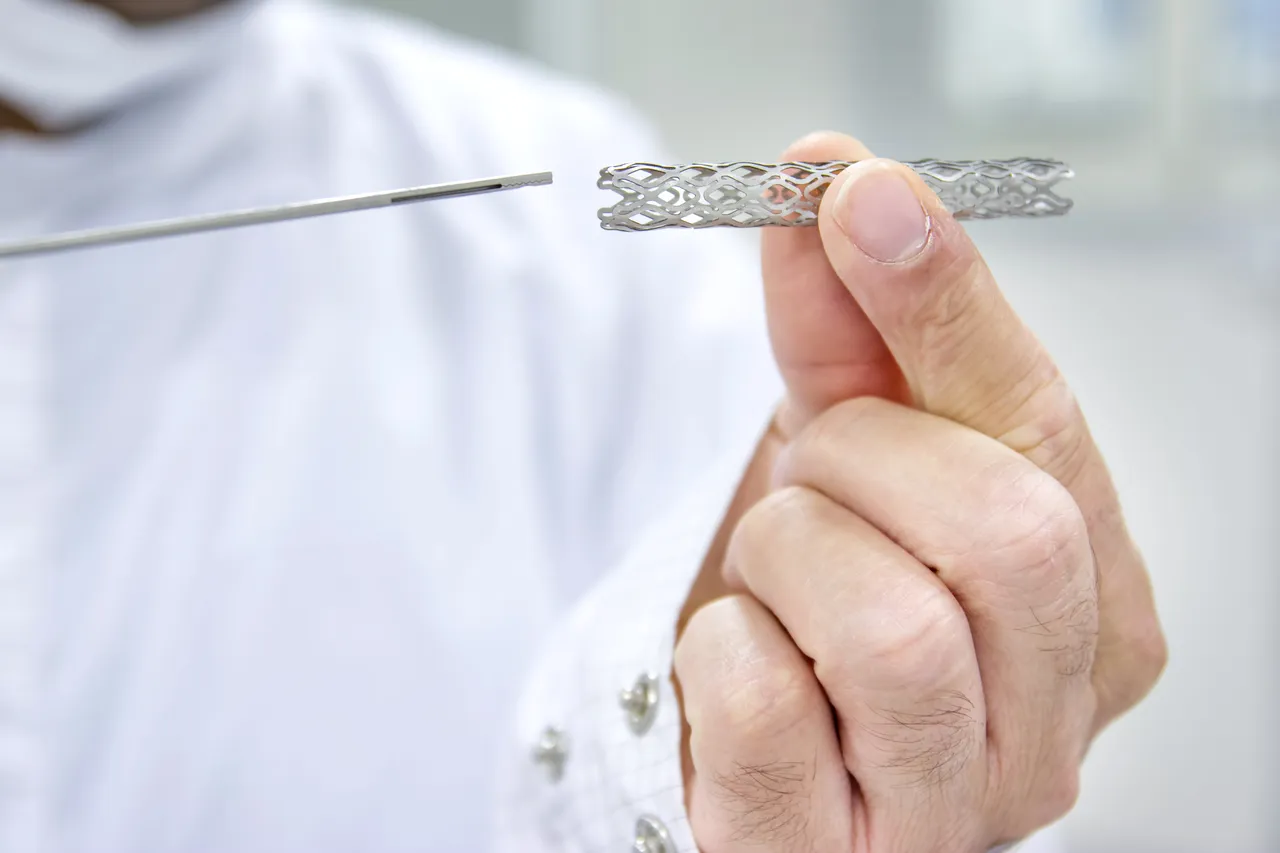
Angioplasty is the part of the procedure that widens a narrowed artery by guiding a small balloon to the affected area and inflating it to improve blood flow. On the other hand, heart stenting involves placing a small metal mesh tube, called a stent, into the artery after it has been widened. The stent provides structural support, helping keep the artery open as it heals and reducing the risk of the artery narrowing again. In many cases, angioplasty and stenting are performed together during the same procedure. However, a stent is not always required.
Your cardiologist may recommend angioplasty, with or without stenting, if:
- You experience recurrent chest pain (angina) despite medication
- Tests show a significant blockage in one or more coronary arteries
- You have had a heart attack and need urgent restoration of blood flow
The decision to proceed, and whether a stent is required, is based on careful assessment of factors such as the location and severity of the blockage, how the artery responds to balloon inflation and your overall health.
What Are the Types of Heart Stents and Their Uses?
Modern cardiology offers different stents, each designed to meet specific needs and patient conditions.
Bare Metal Stents (BMS)
Bare metal stents are the most basic type of coronary stent. They are made from stainless steel or chromium cobalt and do not contain any drug coating. Their primary purpose is to hold the artery open and restore blood flow. Once implanted, bare metal stents remain permanently in the artery and cannot be removed.
Drug-Eluting Stents (DES)
Drug-eluting stents are made from metal frameworks similar to bare metal stents but include an additional drug coating. This medication is gradually released into the artery after implantation to reduce the growth of scar tissue, which can otherwise cause the artery to narrow again. Because this coating significantly lowers the risk of re-narrowing compared with bare metal stents, drug-eluting stents are now far more commonly used today.
Bioresorbable Vascular Scaffolds (BVS)
Bioresorbable vascular scaffolds are a newer type of stent and, unlike bare metal and drug-eluting stents, are not designed to be permanent. They are made from bioabsorbable materials such as magnesium or specialised polymers and are also coated with medication to reduce the risk of re-narrowing. The scaffold provides temporary support to keep the artery open and is designed to gradually dissolve in the bloodstream over approximately two years, leaving no permanent metal behind once the vessel has healed.
How Do I Prepare for Angioplasty With Stenting?
It’s natural to feel a little anxious before a heart procedure, but preparation can help you feel more at ease while knowing you are taking steps to restore your heart health. Your cardiologist will provide personalised instructions, which may include:
- Pre-Procedure Tests Heart Screening: Your cardiologist may recommend a series of tests, including heart screening, blood tests, electrocardiography (ECG) and cardiac imaging to get a comprehensive understanding of your heart’s condition before the procedure.
- Medication Review: Some medications, particularly blood thinners, may need to be paused to reduce the risk of bleeding.
- Fasting: Avoiding food or drink for several hours before the procedure is usually required to prevent complications during sedation.
- Support: Discussing concerns with your doctor or bringing a loved one along can offer reassurance and emotional comfort.
What Are the Potential Complications of Angioplasty With Stenting?
Coronary angioplasty with stenting is generally considered safe, but like all medical procedures, it carries some risks. Possible complications may relate to the angioplasty procedure itself or to the placement of the stent.
Potential complications include:
- Bleeding or bruising at the catheter insertion site
- Allergic reactions to the contrast dye used during imaging
- Re-narrowing of the artery (restenosis) over time
- Formation of blood clots around or within the stent
Your doctor will explain these risks in detail and take appropriate precautions to minimise them, while closely monitoring you throughout the procedure.
Safely Restoring Heart Blood Flow at EH Heart Specialist
Angioplasty with stenting is used to improve blood flow to the heart when narrowed arteries begin to affect daily life or raise the risk of more serious problems. By easing symptoms such as chest pain and restoring circulation, the procedure can help protect the heart muscle and support recovery. When combined with careful assessment, appropriate stent selection, and follow-up care, angioplasty becomes part of a longer-term plan to manage heart disease and help patients maintain an active, healthier life.
At EH Heart Specialist Clinic, angioplasty with stenting is offered as part of a carefully planned approach to restore heart blood flow, relieve symptoms, and protect heart muscle function. Led by Dr Eric Hong, our clinic provides personalised assessment and interventional expertise to determine whether stenting is appropriate, with careful attention to stent selection and long-term heart health. Book an appointment with us today to discuss your symptoms and results, and take the next step towards safer, stronger heart health.
Meet Our Cardiologist
Dr Eric Hong
MB BCh (Ireland), MRCP (United Kingdom) FAMS (Cardiology), DIP (CBNC, USA) FSCAI (SCAI, USA), FACC (ACC, USA) FESC (European Society of Cardiology, France) FRCP (Edinburgh, United Kingdom)

Dr Eric Hong is a dedicated cardiologist in Singapore with over 20 years of experience caring for heart patients.
He is one of few cardiologists in Singapore who subspecialises in interventional cardiology, nuclear cardiology, and multi-modal cardiac imaging. Committed to achieving the best possible outcomes for his patients, heart specialist Dr Eric Hong brings diverse experience from Ireland and the United States, and is double fellowship-trained in the USA.












